Nicholson-funded Collaborative Addresses New Jersey's Prescription Opioid Crisis
The Nicholson Foundation has launched a statewide initiative to help primary care providers better treat chronic pain and reduce their over-reliance on prescription opioids. The New Jersey Pain Care Collaborative (the Collaborative) connects local physicians with nationally recognized experts to learn new techniques for treating chronic pain instead of relying primarily on prescription opioids. To treat their patients who are already opioid-dependent, the Collaborative also increases physicians’ expertise and confidence in using buprenorphine, an FDA-approved medication for managing opioid dependence.
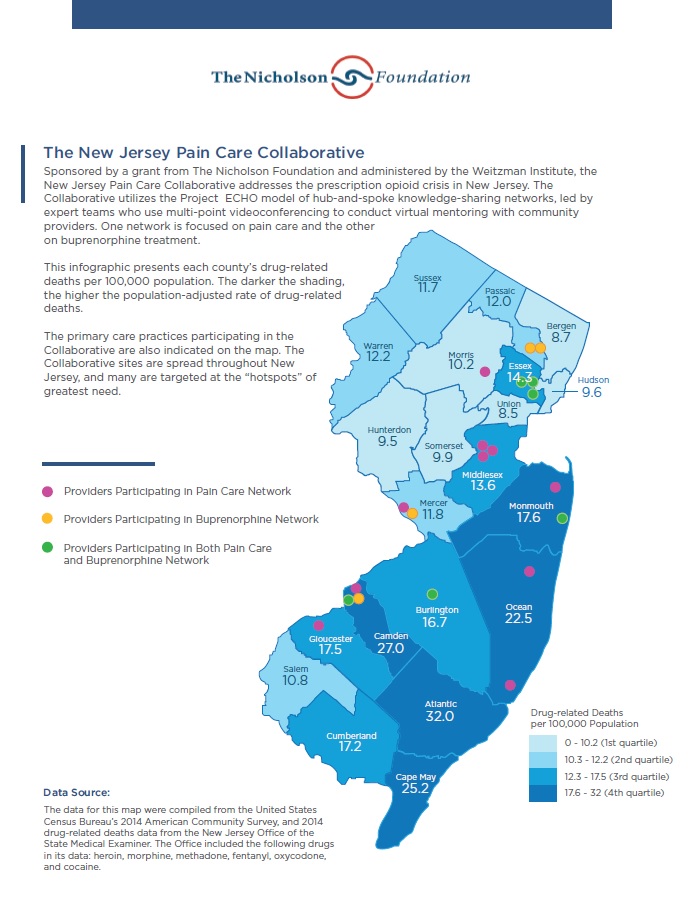
Twenty-nine providers from 20 healthcare practices across New Jersey will participate in the initiative at its launch. By supporting the integration of behavioral health and primary care, the Collaborative builds on previous Nicholson-funded projects to improve care for vulnerable populations in New Jersey. Enhancing the ability of primary care providers to manage substance use disorders will help to reduce costs of care and improve overall health outcomes.
Current prescribing practices are a significant contributor to the opioid overdose epidemic. Primary care providers receive little or no training in how to treat chronic pain, and often rely on prescription opioids. There is little evidence that opioid pain relievers have long-term benefits and they present serious risks of addiction and death from overdose. When compared to other medications for moderate-to-severe pain, they also increase the risk of death from cardiorespiratory and other causes. The Collaborative seeks to reduce the reliance on prescription opioids through a multi-pronged strategy that includes prevention, treatment, and practice transformation.
Functioning through two regularly-scheduled “clinics”—one for pain care and another for buprenorphine treatment—the Collaborative uses web-based videoconferencing to build mentoring partnerships between primary care physicians in New Jersey and interdisciplinary teams of nationally recognized experts. The primary care physicians present case studies of their patients to the experts, who provide feedback, mentoring, and didactic presentations. The clinics are operated by the Connecticut-based Weitzman Institute, and providers will receive Continuing Medical Education credits for participating.
The pain care clinic connects physicians with a team of experts comprised of a pain medicine specialist, clinical pharmacist, psychologist, licensed clinical substance abuse professional, and a specialist in Chinese medicine and acupuncture. The specialists mentor the primary care physicians in methods of pain care that do not involve prescription opioids. In this way, the clinic builds a “community of practice” to help change the prescribing behaviors that have helped to fuel the opioid epidemic.
Ten of the practices participating in the pain care clinic also engage in a practice transformation component. Experienced coaches work with all levels of staff to make the necessary changes in work flow, data collection, and policies and procedures to support physicians in providing evidence-based pain care. Select participating sites also incorporate on-site chiropractic services for pain patients as an evidence-based alternative to prescription opioids.
The buprenorphine clinic connects physicians with a team of addiction experts comprised of a primary care physician, psychiatrist, clinical psychologist, clinical pharmacist, behavioral health clinician, and medical assistant.
At the launch of the Collaborative, twelve communities across New Jersey will have physicians participating. The Collaborative is available for enrollment from new primary care providers—please click here to request information on joining.
Learn More:
Download a Map/Infographic on the Collaborative Sites
Resources on the Opioid Epidemic
Media Coverage: